What is Loeys-Dietz Syndrome?
Loeys-Dietz syndrome (LDS) is a rare genetic disorder that affects the connective tissue in the body. The disorder was first described in 2005 by Dr. Bart Loeys and Dr. Hal Dietz at the Johns Hopkins University School of Medicine.
LDS is caused by a mutation (change) in either the TGFBR1 or TGFBR2 genes (transforming growth factor beta receptor 1 or 2), the SMAD2 or SMAD3 genes (mothers against decapentaplegic homolog 2 or 3), or the TGFB2 or TGFB3 genes (transforming growth factor beta 2 or 3).
There are six genetic causes of Loeys-Dietz syndrome:
- Loeys-Dietz syndrome type 1, caused by mutations in the TGFBR1 gene
- Loeys-Dietz syndrome type 2, caused by mutations in the TGFBR2 gene
- Loeys-Dietz syndrome type 3, caused by mutations in the SMAD3 gene
- Loeys-Dietz syndrome type 4, caused by mutations in the TGFB2 gene
- Loeys-Dietz syndrome type 5, caused by mutations in the TGFB3 gene
- Loeys-Dietz syndrome type 6, caused by mutations in the SMAD2 gene
Loeys-Dietz syndrome is a genetic disorder. The genetic component means that LDS is present in an individual since their conception and that LDS may be passed from parent to child in an autosomal dominant inheritance pattern. This pattern means that each offspring of an individual with LDS has a 50% chance of inheriting the gene mutation for LDS and the condition. There is no way to predict the severity of symptoms that may occur.
Individuals with LDS exhibit a variety of medical features in the cardiovascular, musculoskeletal, cutaneous (skin), immune, and gastrointestinal systems. LDS medical characteristics will vary from person to person, with various combinations of features ranging from mild to severe in presentation.

Four common features of LDS include:
- Aneurysms (widening or dilation of arteries), which can be observed by imaging techniques. These are most often observed in the aortic root (base of the artery leading from the heart) but can be seen in other arteries throughout the body
- Arterial tortuosity (twisting or spiraled arteries), most often occurring in the vessels of the neck and observed on imaging techniques
- Hypertelorism (widely spaced eyes)
- Bifid (split) or broad uvula (the little piece of flesh that hangs down in the back of the mouth)
It’s important to note that that these findings are not observed in all patients and do not concretely lead to a diagnosis of LDS. It is recommended that you consult your physician or a local geneticist if you have questions about individual health concerns.
For a detailed list of symptoms, visit the Loeys-Dietz Syndrome Foundation Canada’s website.
Individuals with LDS are more likely than the general population to experience gastrointestinal issues including eosinophilic esophagitis and gastritis or inflammatory bowel disease.
What is Inflammatory Bowel Disease (IBD)?
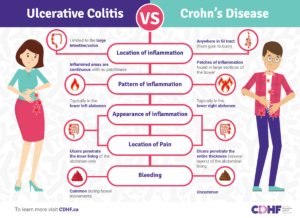
Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of the digestive tract, and is the umbrella term for two, separate disorders that cause inflammation (redness and swelling) and ulceration (sores) of the small and large intestines. These two disorders are called ulcerative colitis and Crohn’s disease. IBD has an enormous impact on affected people, and Canada has one of the highest rates of IBD in the world. IBD can be painful and debilitating and may even lead to life-threatening complications.1
Ulcerative colitis symptoms include:
- Severe and bloody diarrhea
- Bowel urgency and less commonly incontinence
- Abdominal pain and cramping
- Nausea and vomiting
- Decreased appetite
- Weight loss
- Fever
- Anemia
- In some patients: eye, joint, and/or skin symptoms
Crohn’s disease can range from mild to severe. It can develop gradually or come on suddenly, without warning. Symptoms, which vary widely depending on the location of the disease along the digestive tract, may include:2
- Abdominal pain
- Cramping
- Perianal disease,
- Obstructions
- Fistulas
- Diarrhea
- Nausea
- Vomiting
- Reduced appetite
- Weight loss
- In some patients: eye, joint, and/or skin symptoms
How is Loeys-Dietz syndrome related to gastrointestinal issues and IBD?
People with Loeys-Dietz syndrome (LDS) often develop gastrointestinal issues, including food allergies, eosinophilic gastrointestinal disease (eosinophilic esophagitis, gastritis, and colitis), constipation, and inflammatory bowel disease (ulcerative colitis and Crohn’s disease). 3
Compared to the general population, individuals with LDS are more likely to have a food allergy to peanuts, tree nuts, milk, soy, eggs, shellfish, fish, wheat, or other foods. Symptoms of a food allergy may be mild, such as swollen, flushed skin or stomach discomfort and bloating, or more severe, such as hives, uncontrollable cough or wheezing, difficulty breathing, vomiting, diarrhea, severe cramping, dizziness, fainting, or blue fingertips or lips. To diagnose a food allergy, a doctor may use a skin-prick test, blood test, or food elimination diet.
Eosinophilic gastrointestinal disease (EGID) is an inflammation of the gastrointestinal tract, from the esophagus (eosinophilic esophagitis), to the stomach and small intestine (eosinophilic gastritis), to the large intestine (eosinophilic colitis).8 This inflammation can be caused by food allergies. In this case, the gastrointestinal tract contains a greater than normal amount of eosinophils, a type of white blood cell involved in the body’s response to infections and allergies. 8 EGID symptoms include vomiting, diarrhea, nausea, food stuck in the esophagus, trouble swallowing, weightloss, and severe heartburn. A diagnosis can be made through a biopsy of the gastrointestinal tract.4
When it comes to inflammatory bowel disease (IBD), it is estimated that 4.3% of people with LDS have IBD.6While further studies are needed among larger groups of people, preliminary research shows that people with LDS may be more likely than others to develop IBD and that the genetic mutations of LDS types 1 and 2 may be involved in its development.
Management of Gastrointestinal Issues, including IBD
Gastrointestinal concerns, such as IBD, EGID, and issues related to food allergies, may affect people for their whole lives. To reduce the frequency and severity of symptoms, proper management is important and must be tailored to each individual. CDHF and LDSFC recommend working closely with your gastroenterologist and other doctors to come up with a treatment and management plan that works for you. The plan may include medication, dietary changes, the use of a feeding tube, or surgery.
To manage LDS gastrointestinal concerns, it is recommended to7:
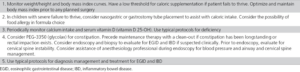
Table: Guidelines for Gastroenterology and Nutrition
Source: MacCarrick, G.; Black III, J. H.; Bowdin, S.; El-Hamamsy, I.; Frischmeyer-Guerrerio, P. A.; Guerrerio, A. L.; Sponseller, P. D.; Loeys, B.; & Dietz, H. C. (2014). Loeys-Dietz syndrome: A primer for diagnosis and management. Genetics in Medicine, 16(8), pp. 576 – 587. DOI: https://doi.org/10.1038/gim.2014.11
To learn more about Loeys-Dietz syndrome and IBD
To learn more about Loeys-Dietz syndrome, visit the Loeys-Dietz Syndrome Foundation Canada.
To learn more about IBD, visit CDHF’s page on Crohn’s disease and on ulcerative colitis.
References
- Coenen S et al. Eur J Gastroenterol Hepatol 2017;29:646.
- Chauhan U et al. J Can Assoc Gastroenterol 2022;5:129.
- MacCarrick, G.; Black III, J. H.; Bowdin, S.; El-Hamamsy, I.; Frischmeyer-Guerrerio, P. A.; Guerrerio, A. L.; Sponseller, P. D.; Loeys, B.; & Dietz, H. C. (2014). Loeys-Dietz syndrome: A primer for diagnosis and management. Genetics in Medicine, 16(8), pp. 576 – 587. DOI: https://doi.org/10.1038/gim.2014.11
- Loeys-Dietz Syndrome: Gastrointestinal issues. Loeys-Dietz Syndrome Foundation. (n.d.). Retrieved October 17, 2022, from https://loeysdietzcanada.org/assets/web/documents/fact_sheets/2019/en/LDSF%20US_Gastrointestinal%20Issues%20Fact%20Sheet_Dec%204%202019.pdf
- Naviglio, S.; Arrigo, S.; Martelossi, S.; Villanacci, V.; Tommasini, A.; Loganes, C.; Fabretto, A.; Vignola, S.; Lonardi, S.; & Ventura, A. (2014). Severe inflammatory bowel disease associated with congenital alteration of transforming growth factor beta signaling. Journal of Crohn’s and Colitis, 8(8), pp. 770 – 774. DOI: https://doi.org/10.1016/j.crohns.2014.01.013
- Guerrerio, A. L.; Frischmeyer-Guerrerio, P. A.; Huang, C.; Wu, Y.; Haritunians, T.; McGovern, D. P. B.; MacCarrick, G. L., Brant, S. R.; & Dietz, H. C. (2016). Increased prevalence of inflammatory bowel disease in patients with mutations in genes encoding the receptor subunits for TGFB. Inflammatory Bowel Disease, 22(9), pp. 2058 – 2062. DOI: https://doi.org/10.1097/MIB.0000000000000872
- MacCarrick, G.; Black III, J. H.; Bowdin, S.; El-Hamamsy, I.; Frischmeyer-Guerrerio, P. A.; Guerrerio, A. L.; Sponseller, P. D.; Loeys, B.; & Dietz, H. C. (2014). Loeys-Dietz syndrome: A primer for diagnosis and management. Genetics in Medicine, 16(8), pp. 576 – 587. DOI: https://doi.org/10.1038/gim.2014.11
- Eosinophilic gastrointestinal disease. Gastrointestinal Society. (2022, August 9). Retrieved October 5, 2022, from https://badgut.org/information-centre/a-z-digestive-topics/eosinophilic-gastrointestinal-disease/