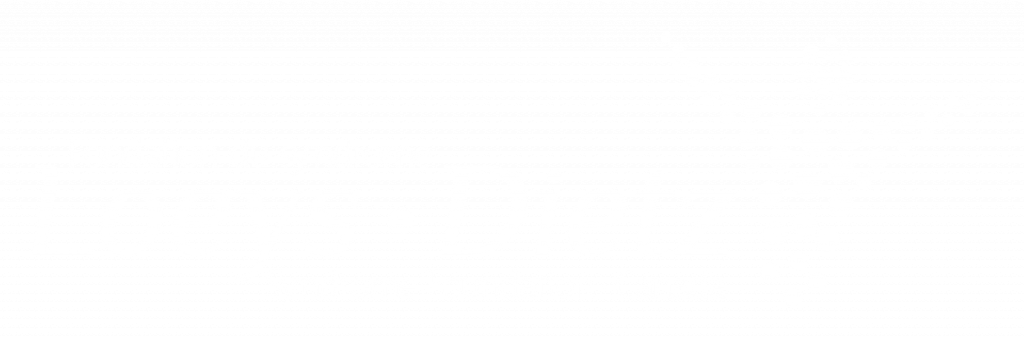
What Is Scoliosis?
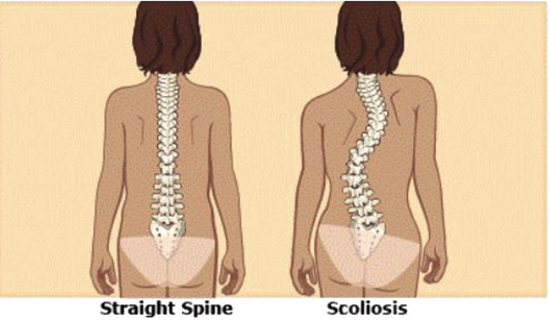
Scoliosis is a spinal deformity that involves both rotation and lateral curvature of the spine The five main types of scoliosis include idiopathic, congenital, neuromuscular, syndrome-related, and scoliosis due to secondary reasons.
- Idiopathic scoliosis is a type of scoliosis where the cause is unknown, or it is not related to a specific syndrome (such as Marfan syndrome), congenital or neuromuscular syndrome.
- Congenital scoliosis is a form of scoliosis which is present from birth. It is theorized to occur due to problems in the development of the vertebrae in-utero.
- Neuromuscular scoliosis is related to a neuromuscular disease (e.g., muscular dystrophy), where the abnormalities in the muscular and/or neurological function result in the curvature of the spine.
- Syndrome-related scoliosis is where the scoliosis is a result of the effects of a disease process, such as Marfan syndrome, Ehlers-Danlos syndrome and Loeys-Dietz syndrome. Due to the mutations in the genes associated with these conditions, it affects the stability of the underlying connective tissue, ultimately leading to scoliosis.
- Scoliosis due to secondary reasons are defined as scoliosis cases where there is a lateral deviation of the spine with minimal rotation of the spine. This could be due to pain, spinal cord abnormalities, tumors or infection.
Scoliosis manifests differently in everyone, and not everyone with scoliosis will look alike.
Impact on Quality of Life
In the majority of cases, scoliosis manifests in childhood, and is usually detected by parents, or by a physician during medical check-ups. In rare cases, scoliosis can manifest in adulthood in a previously healthy spine. The impact of scoliosis on quality of life varies significantly, depending on the degree of curvature, type of scoliosis present, other underlying illnesses, and access to care.
Signs of Scoliosis
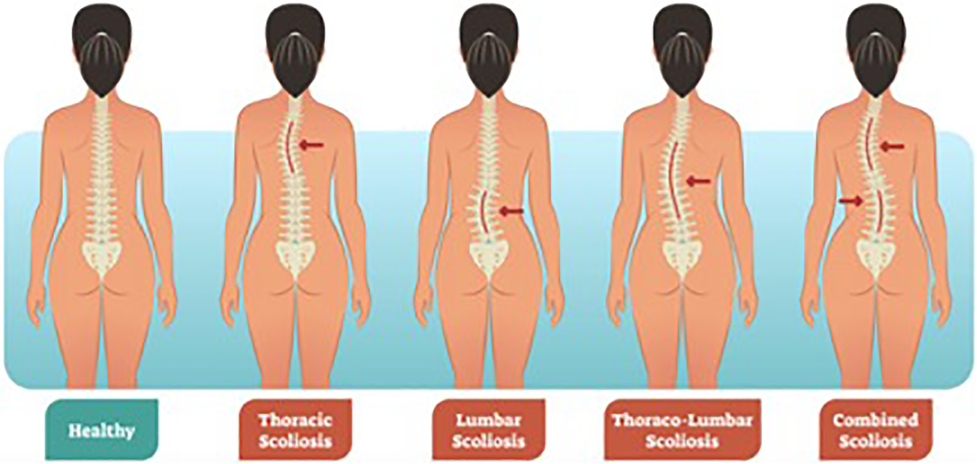
One of the diagnostic tests used for scoliosis is the Adam Forward Bend test, where when the person bends forward, the ribs protrude on one side. In addition, physicians will use x-rays and other diagnostic tools for screening scoliosis.
Image: Adam Forward Bend Test
How Are Connective Tissue Disorders Related to Scoliosis?
When there is co-occurrence of scoliosis with connective tissue disorders such as Loeys-Dietz syndrome (LDS), Marfan syndrome (MFS), and Ehlers-Danlos syndrome (EDS), it falls into the syndromic scoliosis classification.
Intersection Between Scoliosis & Loeys-Dietz Syndrome
Loeys-Dietz syndrome (LDS) is a connective tissue disorder that primarily impacts the cardiovascular, skeletal, and cranio-facial structures. It is reported that 62% of people with LDS also have scoliosis, with it being present in all LDS subtypes.
Intersection Between Scoliosis & Marfan Syndrome
Marfan syndrome (MFS) is a connective tissue disorder involving a mutation in the fibrillin-1 (FBN1) gene, which impacts multiple systems throughout the body. Scoliosis is highly prevalent in those with MFS, where it has been reported that approximately 60% of those with MFS have scoliosis. It has been theorized that there is a higher prevalence of scoliosis in this population due to ligament laxity.
Intersection Between Scoliosis & Ehlers-Danlos Syndrome
Ehlers-Danlos syndrome (EDS) is a connective tissue disorder characterized by mutations that affect collagen. Scoliosis makes up 23% of musculoskeletal complications in those with EDS. Researchers hypothesize that low muscle tone and lax ligaments are the main contributors to scoliosis in this population. While scoliosis is more common in those with kyphoscoliotic EDS (kEDS), hypermobile EDS (hEDS), and classical EDS (cEDS) it can be present in the other types of EDS as well. kEDS has been associated with a particularly severe scoliosis with a rapid progression. On the other hand, hypermobile EDS is associated with mild scoliosis.
Spotlight On Vascular Ehlers-Danlos Syndrome (vEDS)
Vascular Ehlers-Danlos syndrome (vEDS) is the third most common form of EDS. It is characterized by fragility of blood vessels potentially leading to arterial rupture or dissection, bowel perforation, or rupture of other organs in the body. It is reported that approximately 33% of those with vEDS have scoliosis. Specific information about the onset or progression of scoliosis in vEDS has not been reported.
Medical Disclaimer: The information provided here is meant to empower individuals to make informed decisions – it does not, however, replace a reader’s relationship with their doctor. Please speak with a qualified healthcare professional before making medical decisions. Research for LDS, MFS, EDS, & vEDS is ongoing. The Loeys-Dietz Syndrome Foundation Canada is not responsible for the quality of the information or services provided by organizations mentioned on loeysdietzcanada.org, nor do we endorse any service, product, treatment, or therapy.
Treatment of Scoliosis
The treatment for scoliosis involves bracing and surgery. Several factors will impact the management of scoliosis, such as the degree of curve, as well as the maturation of the bone, puberty, and speed of progression of scoliosis. Patients with scoliosis are monitored regularly to track how quickly the curvature is increasing, which will inform the management that is chosen.
Treatments specific to syndromic scoliosis have not been explored, and treatment is focused on bracing, to limit progression of the curvature, and surgery. Research shows that those with connective tissue disorders such as MFS, LDS and EDS, may not respond well to bracing due to underlying ligament laxity. Moreover, curves progress much faster with these conditions, and due to the poor response to bracing, surgery would be the next treatment option. Surgical treatment has led to improvement in function, and improved quality of life in EDS, MFS and LDS.
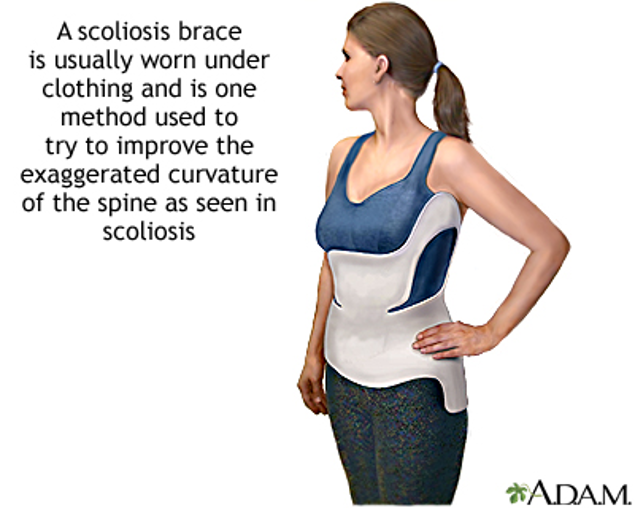
Image: Brace used for scoliosis treatment.
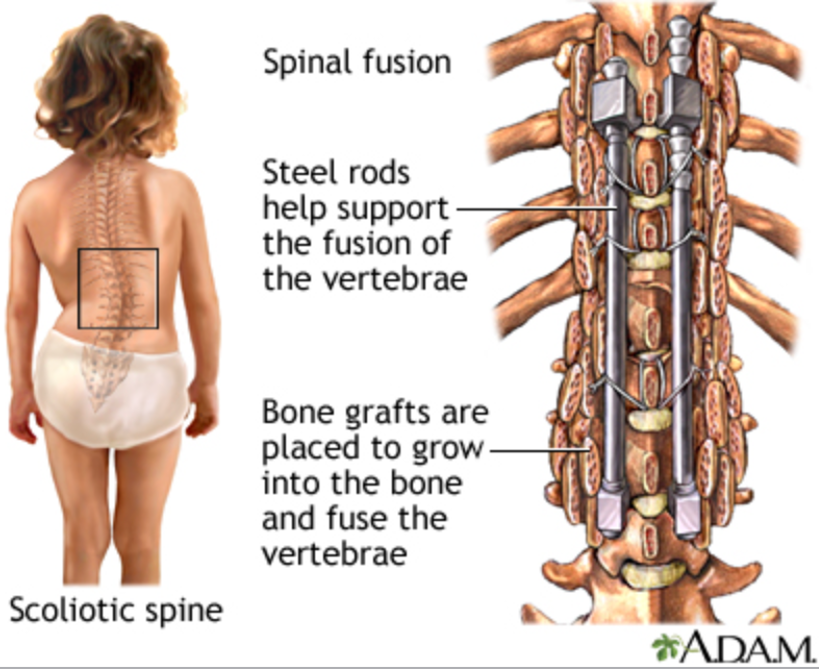
Image: Surgical correction of the spine in scoliosis.
Surgical Complications in Scoliosis Treatment
If you are considering surgery, please talk to your doctor about any associated risks and how to best prepare for them.
Surgical treatment may carry an increased risk of complications for those with LDS, EDS and MFS, such as blood loss due to tissue fragility. Also, cerebrospinal fluid leaks and additional revision surgeries are complications reported in LDS and MFS patients.
Furthermore, those with connective tissue disorders may have different anesthesia needs, and staying informed can aid in patient advocacy, and makes the journey as comfortable as possible. There are many clinicians, physicians and surgeons who are aware of these unique needs and take extra measures to minimize complications.
To learn more about preparing for surgery for someone with Loeys-Dietz Syndrome, please visit (https://loeysdietzcanada.org/patient-support/preparing-for-surgery/#elementor-toc__heading-anchor-5).
Anderson, P., & Peters, R. (2023). Surgical considerations for patients with Loeys-Dietz syndrome and scoliosis. JAAOS Global Research & Reviews, 7(3), e00061. https://doi.org/10.5435/JAAOSGlobal-D-23-00061
Brown, L., & Williams, D. (2012). Diagnosis and management of Loeys-Dietz syndrome: A case study. New England Journal of Medicine, 367(2), 190-198. https://doi.org/10.1056/NEJMcp1209063
Chang, A., & Manz, J. (2021). Genetic basis of Loeys-Dietz syndrome: A review of the mutations and molecular mechanisms. Genes, 14(6), 1173. https://doi.org/10.3390/genes14061173
Chen, M., & Patel, S. (2019). Clinical management of Loeys-Dietz syndrome and its cardiovascular implications. Journal of Cardiovascular Disease, 22(10), 1234-1242. https://doi.org/10.1177/1559325819852810
Elder, R. H., & Von Baeyer, C. L. (2009). Chronic pain in children and adolescents: An overview. Pediatric Clinics of North America, 12(9), 771–789. https://doi.org/10.1093/pch/12.9.771
Garfin, S. R., & Bohlman, H. H. (2012). Current concepts in the management of spinal deformity. Orthopaedic Clinics of North America, 43(4), 653–662 https://doi.org/10.1016/j.otsr.2012.11.002
Gillas, F., Mekki, A., Foy, M., Carlier, R., & Benistan, K. (2021). Prevalence of scoliosis in hypermobile Ehlers-Danlos syndrome. European Medical Journal, 54–62. https://doi.org/10.33590/emj/20-00284
Johnson, E., & Long, M. (2023). Loeys-Dietz syndrome and its skeletal manifestations: A clinical report. Cureus, 15(2), e36372. https://doi.org/10.7759/cureus.36372
Kumar, R., & Gupta, R. (2008). Scoliosis in a child with Loeys-Dietz syndrome. Pediatric Clinics of North America, 12(9), 771–773. https://doi.org/10.1093/pch/12.9.771
Lee, S., & Park, K. (2020). Comprehensive approach to managing scoliosis in connective tissue disorders. Nursing Practice Journal, 41(8), 1132-1140. https://doi.org/10.1016/j.nurpra.2019.08.017
Meester, J. A. N., Verstraeten, A., Schepers, D., Alaerts, M., Van Laer, L., & Loeys, B. L. (2017). Differences in manifestations of Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome. Annals of Cardiothoracic Surgery, 6(6), 637–64 https://doi.org/10.21037/acs.2017.11.03 Menger, R. P., & Sin, A. H. (2025). Adolescent idiopathic scoliosis. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499908/
National Institutes of Health. (2020). Loeys-Dietz syndrome: A comprehensive overview. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK1133/ National Institutes of Health. (n.d.). Scoliosis. In Adam Medical Encyclopedia. U.S. National Library of Medicine. Retrieved April 29, 2025, from https://ssl.adam.com/content.aspx?productid=10&isarticlelink=false&pid=10&gid=000068&site=makatimed.adam.com&login=MAKA1603
Patel, V., & Khan, S. (2022). Cardiovascular manifestations in Loeys-Dietz syndrome: Diagnosis and management. International Journal of Cardiology, 375, 135–143. https://doi.org/10.1016/j.ijcard.2022.05.065
Prabhakar, G., Gonuguntla, R. K., Momtaz, D., Chaput, C., & Hogue, G. D. (2023). Vascular injury after scoliosis correction in Ehlers-Danlos Syndrome: Proceed with caution. JAAOS: Global Research and Reviews, 7(8). https://doi.org/10.5435/jaaosglobal-d-23-00061
Sanchez, J. M., & Newton, J. A. (2003). The efficacy of nonoperative treatment for degenerative disk disease. European Spine Journal, 12(5), 469–474. https://doi.org/10.1007/s00586-003-0555-6
Smith, J., & Harris, D. (2014). Long-term follow-up of Loeys-Dietz syndrome: Implications for the management of scoliosis and vascular health. Spine, 39(7), 1595–1600. https://doi.org/10.1097/BRS.0b013e31818d58da
Wilson, J., & Thomas, H. (2019). Loeys-Dietz syndrome: A genetic overview and clinical implications. Pediatric Orthopedics, 35(4), 199-205. https://doi.org/10.1097/BPO.0000000000000833
Zhang, Z., & Zhao, Q. (2019). Current perspectives on Loeys-Dietz syndrome. CMAMD Journal, 11(6), S10279. https://doi.org/10.4137/CMAMD.S10279